What does hope sound like in a clinical note?
In a small outpatient clinic outside Seattle, Dr. Ramirez scanned a routine follow-up note. Her patient, a 17-year-old girl recently prescribed asthma medication had seemed stable. But embedded in the note was a phrase: “She says it’s becoming harder and harder to take her medication because sometimes she feels like a weirdo among her friends.” A flag lit up. The clinic’s AI assistant, powered by John Snow Labs’ NLP models, detected the language as a possible indicator of low self-esteem and emerging depression.
That flag wasn’t just a red highlight. It was a second set of eyes. And it changed the patient’s care.
Why are so many mental health symptoms going unnoticed?
Mental illness affects one in five adults in the U.S., yet over 60 million mental health-related visits often go undercoded, undertracked, and underestimated. The problem isn’t a lack of data, it’s where the data hides. Structured fields in electronic health records (EHRs) rely on billing codes. They miss the nuance of free-text notes, where a nurse might write, “The child seems more withdrawn,” or a parent might report, “He’s been irritable since starting new meds.”
These clues don’t show up as ICD-10 codes. But they live in the language.
What happened when AI read between the lines?
The MOSAIC-NLP project, funded by the FDA Sentinel Innovation Center, brought together John Snow Labs, Oracle Health, and children’s hospitals across the U.S. They use NLP to detect neuropsychiatric side effects of montelukast, a common asthma medication. When researchers applied AI to over 17 million clinical notes, the number of detected suicidality and self-harm events doubled compared to structured data alone.
Real outcomes hid in plain sight, until machines learned to read like clinicians.
How does Conversational AI step in before crisis?
AI doesn’t just analyze; it talks. Tools like Aiberry and Limbic Access now screen patients via short conversations, interpreting facial expressions, speech patterns, and word choice.
In one U.S. hospital system, a chatbot flagged a patient’s late-night journal entry in a support portal. “I don’t think I matter.” The system escalated the case. A clinician followed up. Intervention replaced isolation.
Can AI understand emotional nuance?
John Snow Labs’ Suicide Detection Social Media model was trained on the raw, unfiltered posts people share when they think no one’s watching. It detects intent, subtle distress, and contextual clues that might otherwise be missed, especially in youth populations. Combined with sentiment analysis and named entity recognition, this AI doesn’t just see words. It understands emotional tone, patterns over time, and urgency.
And unlike a human therapist, it never sleeps.
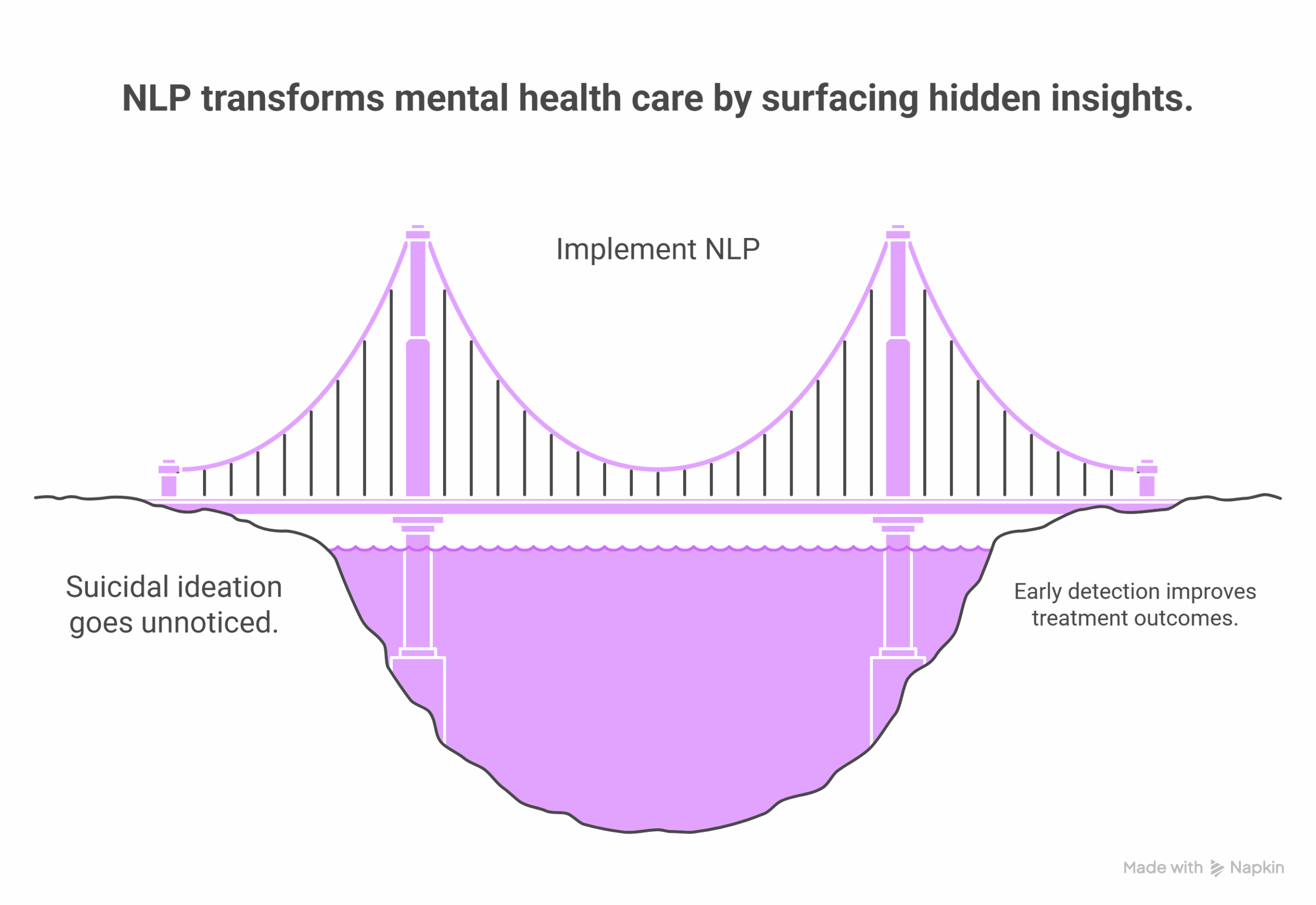
How is NLP transforming mental health care, quietly?
The transformation isn’t loud. It’s incremental. A clinician notices a pattern. A parent gets a phone call earlier than expected. A chatbot provides reassurance to someone at 2 a.m. Behind the scenes, NLP systems are:
- Surfacing suicidal ideation that would be missed in structured fields
- Flagging irritability, memory loss, or behavioral changes
- Distinguishing between affirmed and negated symptoms in notes
- Supporting treatment plans with psychiatric-specific language models
In the MOSAIC-NLP study, behavioral signs in children,”tantrums at school,” “refuses to sleep alone” were classified by AI models even when no formal diagnosis was given. It’s the kind of insight that can shorten the time from observation to action.
Why does this matter now?
Mental health care faces a supply-demand crisis. There are too few providers for too many needs. Yet with tools like John Snow Labs’ Healthcare NLP, health systems gain an invisible ally. These AI models turn unstructured data into clinical insight, whether for real-time alerts or retrospective research.
And for the 17-year-old who “felt like a weirdo”, that insight led to a counseling referral. The next visit told a different story.
“I’m feeling better. I started talking to someone.”
The words were small. But this time, they weren’t missed.
FAQs
Can NLP detect suicidal ideation before a diagnosis is made?
Yes. In the MOSAIC-NLP study, NLP doubled the identification of suicidality and self-harm events from clinical notes.
Is this technology used in real clinics today?
Yes. NHS England uses AI-powered triage tools like Limbic Access, and several U.S. hospital systems have integrated AI into support portals and EHRs.
What makes pediatric mental health detection harder?
Symptoms often present as behaviors, not words. NLP trained on pediatric language can recognize distress in phrases like “screaming when separated.”
Can AI replace therapists?
No. It supports them, by reducing missed symptoms, flagging risk, and expanding access during gaps in care.