Why is clinical documentation driving burnout?
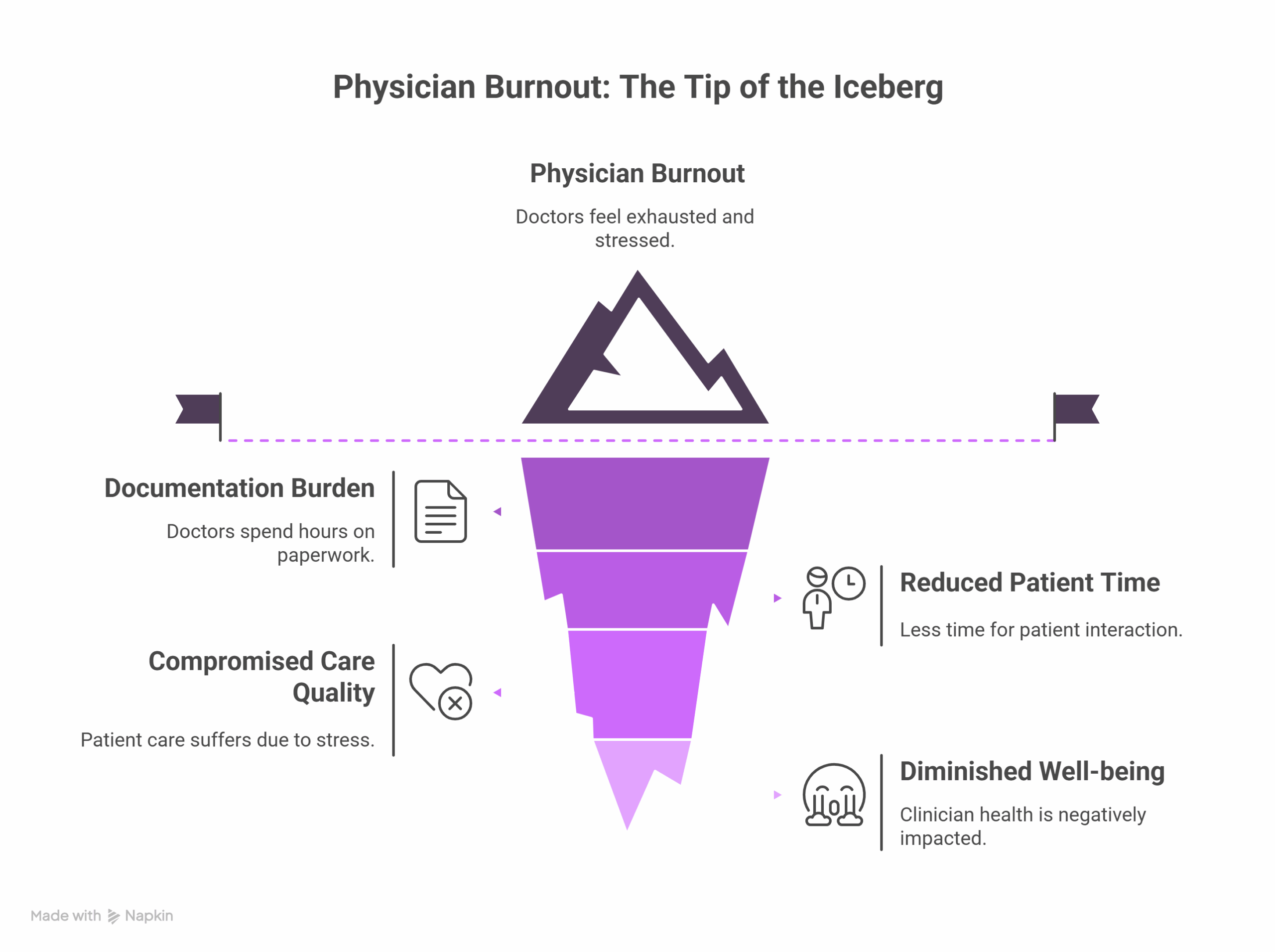
Documentation is one of the most cited contributors to physician burnout. Doctors are spending hours outside of clinic, often termed “pajama time”- finishing notes, reducing time for patients and family. This growing administrative burden compromises both clinician well-being and care quality.1
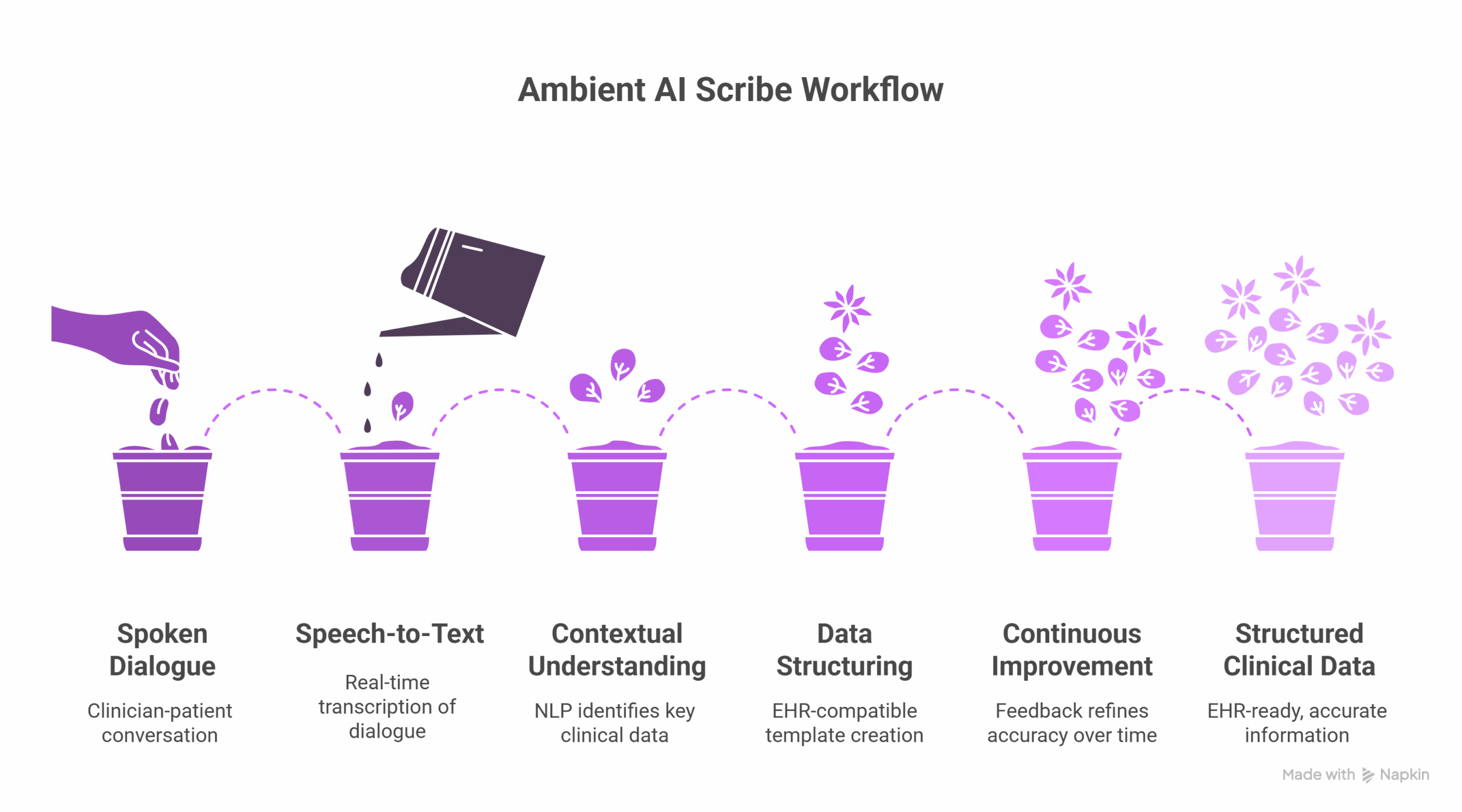
What are ambient AI scribes and how do they work?
Ambient AI scribes are intelligent systems that passively listen to patient-provider conversations and generate clinical documentation in real time. These systems rely on advanced speech recognition, natural language processing (NLP), and large language models (LLMs) to create structured, compliant clinical notes with minimal disruption to the provider’s workflow.
What NLP capabilities power ambient AI scribes?
Ambient scribes integrate multiple core healthcare NLP functions. First, speech-to-text transcription converts spoken dialogue into text in real time with high accuracy. Next, contextual understanding powered by NLP models identifies and categorizes key clinical information such as symptoms, diagnoses, and treatment plans. The system then structures transcribed data into EHR-compatible templates that support both coding and compliance needs. These AI scribes continuously improve through feedback from clinicians, which refines their accuracy and customization over time.
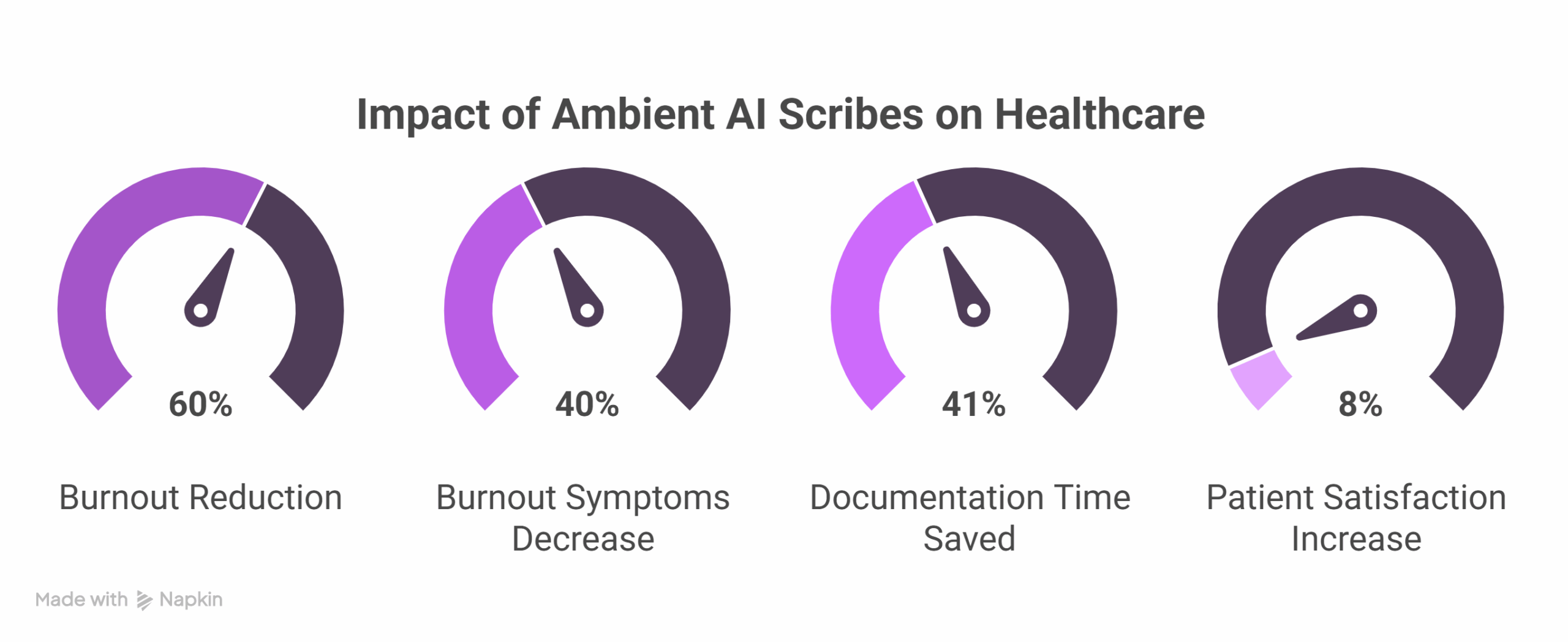
How do ambient AI scribes reduce burnout and improve care?
The introduction of ambient scribes brings measurable improvements to both provider wellness and patient satisfaction. Studies show that up to 60% fewer primary care physicians report burnout after using AI scribes, and some health systems have observed a 40% decrease in burnout symptoms2. Documentation time can be reduced by 41%3, saving clinicians nearly an hour each day. These time savings also translate to improved patient experience, with 8% higher satisfaction scores due to more face-to-face interaction during visits4.
Where are ambient scribes being used, and what are the challenges?
These solutions are being deployed across primary care, specialty clinics, and even in nursing workflows. However, there are several challenges. Integrating with existing electronic health record systems can be complex. Compliance with HIPAA regulations demands strong data protection and privacy safeguards. Hardware setup, including microphone quality and secure environments, is critical for optimal performance. Clinician trust is also essential, and depends on the transparency, accuracy, and perceived value of the system5.
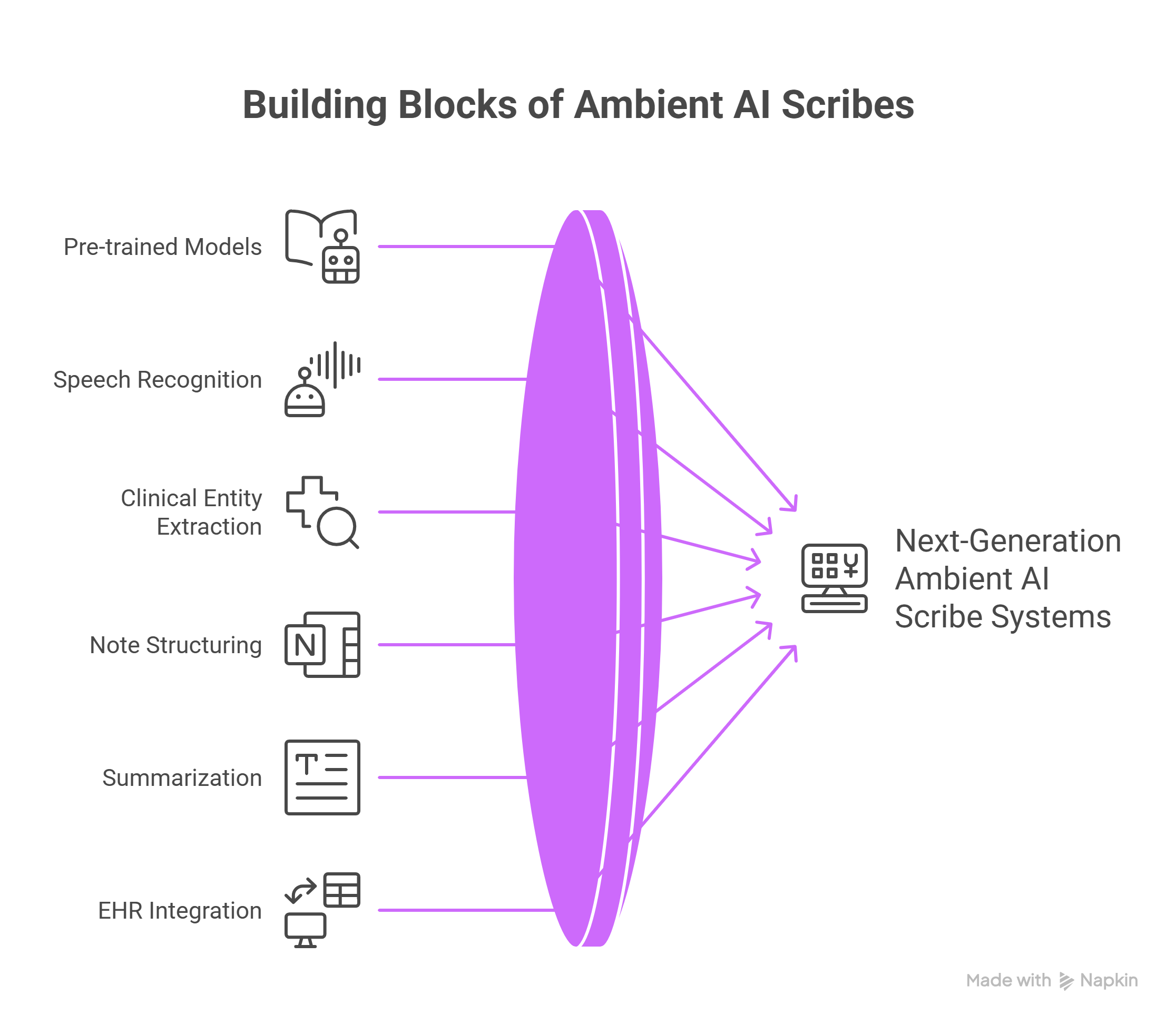
What does the future of ambient AI scribes look like?
The next generation of ambient scribes is set to expand well beyond transcription. Predictive documentation will leverage real-time signals to anticipate needs during the clinical encounter. Fully autonomous scribing may become viable in lower-risk contexts, reducing the need for human review. These scribes will increasingly integrate into broader digital ecosystems, supporting decision-making tools and analytics platforms. Research continues to evaluate long-term return on investment and scalability for broader implementation.
How can John Snow Labs’ Healthcare NLP be used to build ambient scribe solutions?
John Snow Labs’ Healthcare NLP platform offers the foundational building blocks necessary for developing ambient scribe technologies. With over 2,000 pre-trained models, it enables real-time speech recognition, clinical entity extraction, note structuring, and summarization tailored for medical workflows. These models are optimized for high accuracy and can be fine-tuned with feedback from healthcare providers, enhancing contextual awareness and adaptability over time. When deployed within a HIPAA-compliant, privacy-first framework, John Snow Labs’ NLP tools support seamless EHR integration, accurate medical documentation, and scalable automation, making them ideal components for building next-generation ambient AI scribe systems.
Conclusion: Why ambient AI scribes are more than just documentation tools
Ambient AI scribes represent a transformative leap in healthcare documentation. They restore the human side of care by minimizing administrative overload, strengthening patient-provider relationships, and supporting sustainable, high-quality clinical environments. As NLP and AI capabilities continue to evolve, these tools are set to become indispensable allies in the delivery of modern care.
FAQs
How do ambient AI scribes differ from traditional medical scribes?
Ambient AI scribes work passively without requiring direct input during the clinical encounter. Unlike human scribes, they operate in real time, leveraging NLP and LLMs to auto-generate structured notes.
Are ambient scribes safe and HIPAA-compliant?
Yes. Leading vendors build their solutions with HIPAA and data privacy frameworks in mind, using encryption and secure access protocols.
Do doctors still review AI-generated notes?
In most settings, clinicians review and edit the draft note before signing. As trust and accuracy improve, the need for edits may decrease.
Can ambient AI scribes integrate with all EHRs?
Integration depends on the vendor and the EHR platform, but many solutions are built to work with major systems like Epic, Cerner, and Allscripts.
What’s next for ambient AI scribes?
Expect more predictive features, deeper analytics integration, and improved contextual awareness to support proactive care.
Supplementary Q&A
How soon do clinicians notice time savings with ambient scribes?
Most providers report immediate time savings after deployment. On average, users reclaim 45 to 60 minutes per day previously spent on documentation tasks.
Can ambient scribes be used in non-physician settings?
Yes. These tools are increasingly being applied to nursing workflows, allied health professionals, and telehealth consults to extend efficiency benefits beyond physicians.
What are the costs and ROI expectations?
While upfront costs vary by vendor and deployment size, many health systems report breaking even within 12 to 18 months due to labor savings and workflow improvements.