Why hospitals must be rebuilt around AI, not merely transformed
Healthcare institutions are facing increasing pressures: workforce shortages, cost constraints, regulatory complexity, and digitally empowered patients. In this context, superficial “digital transformation” in the form of automation of existing workflows with legacy systems will not be enough. Instead, successful hospitals will rebuild themselves around AI‑native platforms, re‑architecting processes, data flows, and decision‑systems to center on intelligent, real‑time, integrated care.
This is not about plugging AI into old systems; it is about establishing AI‑centric infrastructure, workflows, and organizational culture that enable continuous learning, proactive care and scalable decision‑support.
What does rebuilding around AI require?
- Data & infrastructure re‑imagined
- Unified data architecture that ingests EHR, imaging, lab, genomic, and patient‑generated data in near‑real time.
- AI‑ready pipelines where data is cleaned, annotated, de‑identified/pseudonymised, versioned, and traceable from source to model output.
- Interoperability standards (as FHIR) embedded and exploited by AI systems.
- Compute and model infrastructure integrated into hospital operations (on‑premise/private‑cloud) enabling low‑latency inference and clinician‑workflow integration.
- Workflows redesigned rather than optimized
- Instead of automating the same tasks faster, workflows are redesigned: e.g., triage systems that proactively route patients based on AI‑predicted risk.
- Decision‑support becomes embedded: clinicians and care teams work with AI engines seamlessly.
- Human‑in‑the‑loop becomes a standard: AI suggests, clinician verifies.
- Documentation, reporting, quality metrics all flow from AI‑augmented processes so manual steps are reduced to a minimum.
- Organizational culture and roles evolve
- Clinicians become supervisors of AI‑systems: verifying and refining rather than interpreting images or notes manually.
- Data scientists, model engineers, and clinical informaticists integrate into care teams.
- Quality, compliance, and safety become continuous lifecycle functions of AI‑systems rather than periodic audits.
- Crafting trust, explainability, and human-AI collaboration becomes strategic imperatives.
How John Snow Labs enables hospitals to rebuild around AI
John Snow Labs provides a full‑stack ecosystem tailored for healthcare institutions undergoing this rebuild:
- Healthcare data pipelines & de‑identification: Platforms that handle ingestion from EHR, imaging, genomics, text; de‑identify or anonymize data; maintain audit logs and data lineage.
- Task‑based NLP & structured extraction: Pre‑built pipelines for converting clinical text (notes, reports, radiology) into structured fields, enabling downstream AI reasoning.
- Vision‑language & multimodal reasoning: While not focusing on a single model, John Snow Labs supports multimodal workflows combining image + text + structured data, enabling hospitals to embed imaging logic into clinical decision loops.
- Generative AI Lab & model orchestration: A no‑code platform that enables chaining of data pipelines, model inference, human‑in‑the‑loop review, monitoring and versioning, ideal for hospitals adopting AI‑native workflows.
- Compliance, auditability & change‑control frameworks: Infrastructure and best‑practice to ensure transparency, documentation, traceability and versioning, elements that are foundational for large‑scale hospital AI deployment.
By leveraging this ecosystem, hospitals can move from patchwork automation toward truly AI‑centric operations, where data, models and workflows are designed from day‑one for intelligence, not retrofitted for it.
What immediate benefits emerge from AI‑centric hospital architectures
- Proactive care delivery: Risk predictions trigger care pathways preventing resources overload and improving outcomes.
- Operational agility: Real‑time supply‑chain, staffing and bed‑utilization decisions become model‑driven rather than reactive.
- Clinician productivity and satisfaction: With AI handling data‑processing, extraction, and routine interpretation, clinicians focus on patient interaction and higher‑level decisions.
- Quality and safety improvement: AI‑driven monitoring and alerting systems reduce lapses, support continuous improvement and detect deviations in real time.
- Scalable innovation: Hospitals can continuously iterate on models and workflows, deploying new use‑cases with lower marginal cost, rather than one‑off projects.
How to begin the rebuild: a strategic roadmap
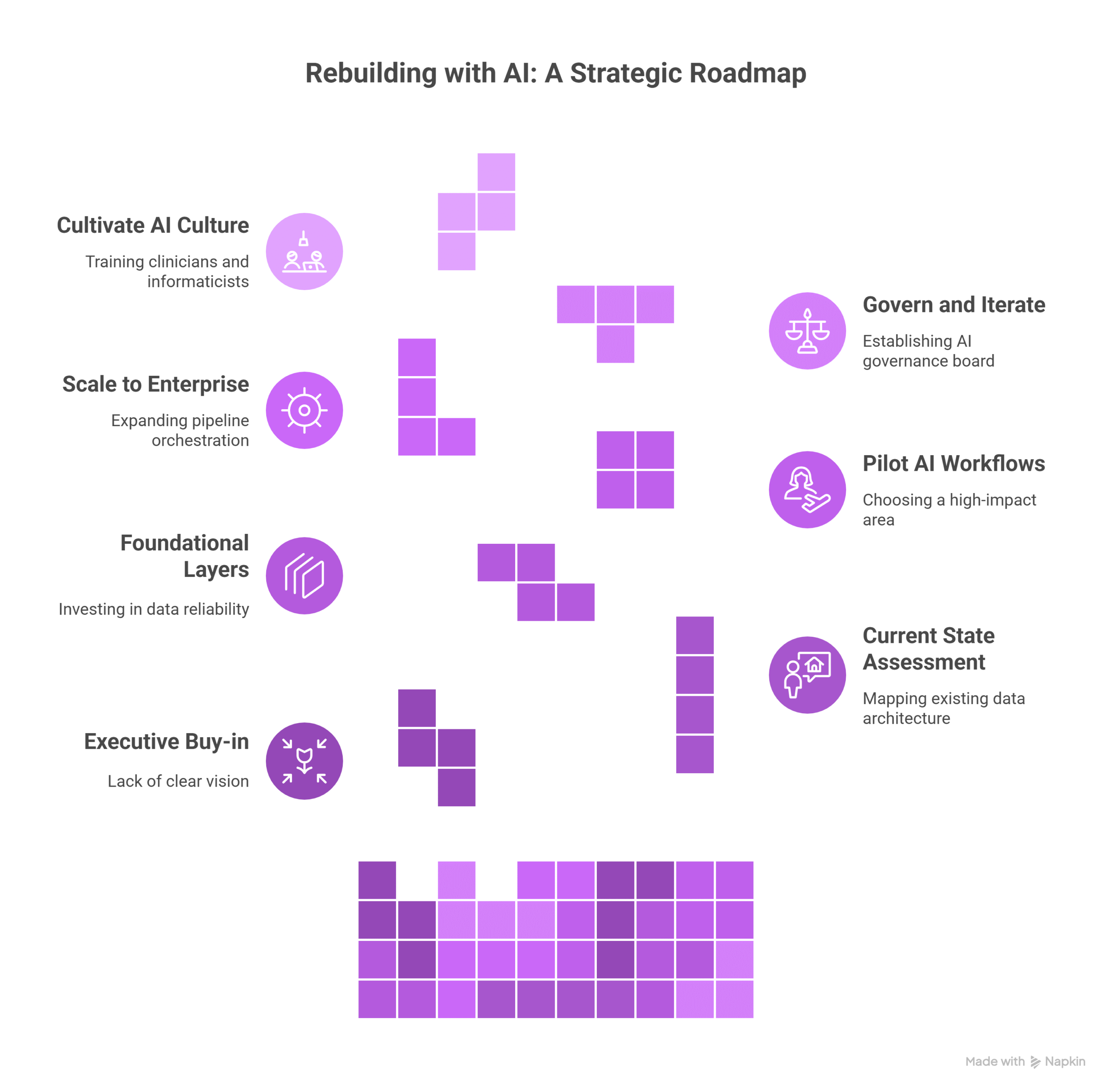
- Executive buy‑in and vision setting: Define what “AI‑centric hospital” means for your organisation: outcomes, capabilities, culture.
- Assess current state & gaps: Map existing data architecture, workflows, staffing, model usage, integration points. Identify bottlenecks and isolations.
- Build foundational layers first: Invest in data reliability, governance, pipelines, interoperability. Without these, advanced AI workflows will fail.
- Pilot AI‑native workflows in visible domains: Choose a high‑impact area (e.g., readmission reduction, imaging triage, registry automation) and build full-stack end‑to‑end proof‑point.
- Scale to enterprise and embed operations: Once proven, expand pipeline orchestration, model governance, human‑in‑the‑loop frameworks, and embed into standard care operations.
- Govern & iterate as organisational capability: Establish AI governance board, model lifecycle management, audit logs, and continuous measurement of outcomes, safety and usage.
- Cultivate AI‑first culture: Train clinicians, informaticists and care teams not just to use AI, but to collaborate with it, refine it and evaluate it.
What happens if hospitals wait or only partially adopt?
- Implementing AI in silos (e.g., one department, one model) without re‑architecting workflows leads to fragmentation, duplicated systems and low ROI.
- Hospitals may fall behind competitors that leverage AI for efficiency, quality, patient experience and staff empowerment, risking margin erosion and market displacement.
- Workforce dissatisfaction increases if clinicians see “AI projects” that add data burden but don’t change workflows.
- Investment in legacy systems may become stranded assets as AI‑centric competitors leap ahead.
Conclusion: This is not incremental transformation, it’s a rebuild
Hospitals that survive and thrive in the coming decade will treat AI not as an add‑on but as the foundation of their operational, clinical and organizational strategy. Building from the ground up, data, workflows, culture and governance, is imperative.
With John Snow Labs’ tools hospitals get a practical path to rebuild around AI rather than being left behind by it.
FAQs
Q: Does “rebuilt around AI” imply replacing all human clinicians?
A: No. The human role remains central. What changes is how clinicians work, shifting from manual data‑processing and routine interpretation toward oversight, exception‑handling and patient‑centric care, supported by AI.
Q: Is it necessary to replace existing EHRs and systems to rebuild?
A: Not necessarily. The rebuild is about layering AI‑native pipelines and integrating workflows. Legacy systems may remain, but the architecture around them must evolve for AI‑centric operation.
Q: How long does the rebuild journey take?
A: It depends on the institution’s maturity and ambition. Pilots can launch in 6‑12 months, but enterprise‑wide AI‑centric transformation typically spans 2‑4 years with phased rollout, governance and capability building.





























