Julia sat quietly, holding a printed brochure about diabetes care while her doctor talked through the usual tips she had heard many times before. At sixty-five, newly widowed and living on her own, she manages both diabetes and high blood pressure. The clinic visit is comforting yet frustrating. She keeps hearing the same broad advice: eat healthier, exercise, and check your sugar. But that advice feels far from her daily life and leaves her feeling lonely rather than helped. Her doctor looks frustrated too, aware that the guidance is too general but pressed for time and short on tools.
Brochure About Diabetes
Living Well With Diabetes
Diabetes is a condition in which the body has trouble using sugar for energy. When sugar stays too high in the blood, it can damage the heart, kidneys, eyes, and nerves. The good news is that steady routines, healthy eating, regular activity, and the right medicines, keep blood-sugar levels closer to normal and protect long-term health.
Why Blood-Sugar Checks Matter
Glucose meters show day-to-day trends. A regular A1C blood test, done in the clinic, tells how well sugar has been controlled over the past three months. Keeping these numbers in range reduces the risk of heart disease and stroke.Healthy Eating Made Simple
Choose whole grains, lean protein, vegetables, fruit, and low-fat dairy at most meals. Limit sugary drinks, sweets, fried food, and large portions. Reading food labels, planning menus, and cooking at home help you stay on track.Move Your Body
Aim for at least 150 minutes of moderate activity each week—this can be brisk walking, cycling, or dancing. Physical activity lowers blood sugar, improves mood, and strengthens the heart.Take Your Medicines on Time
Many people use pills such as metformin or medicines you inject. Follow the schedule your doctor gives. Never stop a medicine without talking to your care team.Watch for Low or High Sugar
If sugar falls too low, you may feel shaky, sweaty, or confused—treat with quick sugar, such as juice. If it stays high, you may feel very thirsty or need to urinate often—call your clinic for advice.Stay Connected
Regular visits with your healthcare team, eye exams, foot checks, and dental care all play a part. Bring questions to every appointment so concerns are handled early.This scene is familiar to many healthcare professionals. Their job is to make sure patients like Julia receive help that fits their lives. Turning clinical guidelines into actions that respect social, financial, lifestyle, and mental factors is hard. When messages stay generic, health suffers, and performance goals slip.
A robust body of research1 demonstrates a clear and positive correlation between personalized patient communication and improved adherence to medical treatments. By moving beyond generic instructions, healthcare providers can significantly enhance the likelihood that patients will follow their prescribed regimens, leading to better health outcomes and more efficient healthcare delivery.
The rise of digital health has opened new avenues for personalized patient communication. Meta-analyses of digital interventions, including text message reminders, mobile apps, and patient portals, have demonstrated their effectiveness in improving medication adherence2. These tools can be highly personalized, delivering timely reminders, educational content, and motivational messages tailored to the patient’s specific needs and schedule. Studies have shown that even simple interventions like personalized text messages can significantly reduce non-adherence.
AI to the rescue, but is it enough?
Technology companies now market artificial‑intelligence services that claim to improve patient communication. Most of these products rely on large language models (LLMs) combined with basic Retrieval‑Augmented Generation. They can write easy-to-read educational notes and send them quickly. Yet these broad systems still miss the mark. A note to Julia might say, “Take a daily walk and buy fresh produce,” without considering her aching knees, tight budget, or the absence of a grocery store near her home. Advice like that can confuse or discourage. Because the models were trained on open‑web text, they ignore many clinical and social details. Errors, conflicting instructions, and blind spots often follow, leaving patients less, not more, supported.
Can we personalize patients’ communications in a better way?
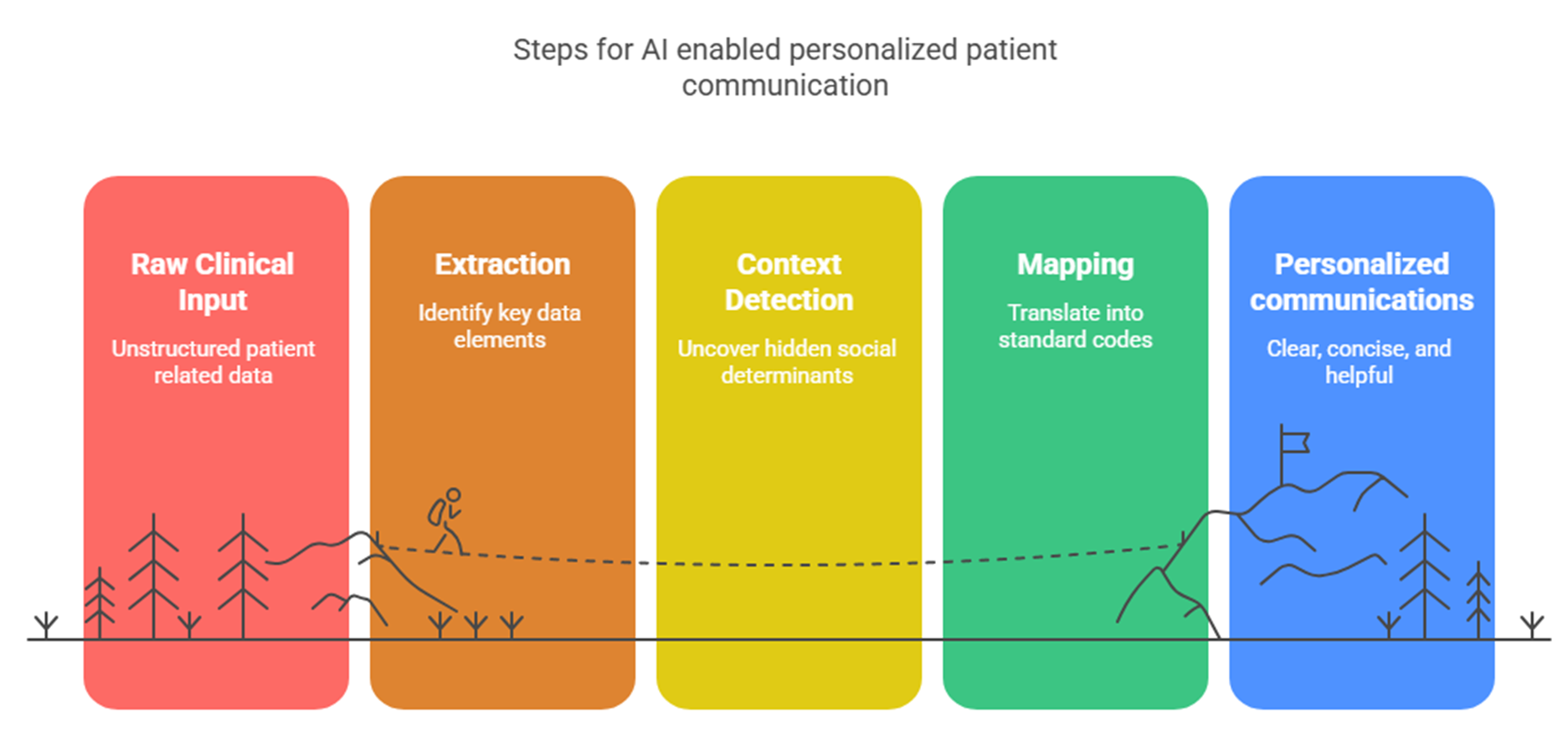
Over the last year, many health systems and research groups have adopted a different approach: pair a medical‑tuned language model with smart and proven natural language processing steps. A Mayo Clinic pilot rewrote discharge notes only after extracting key facts as diagnoses, medications, and follow-up tasks, using rule‑based NLP3. Stanford University reported similar gains when it combined medical transformers with pipelines that detect social needs in free text4. These studies show that context‑aware systems outperform one‑size‑fits‑all bots.
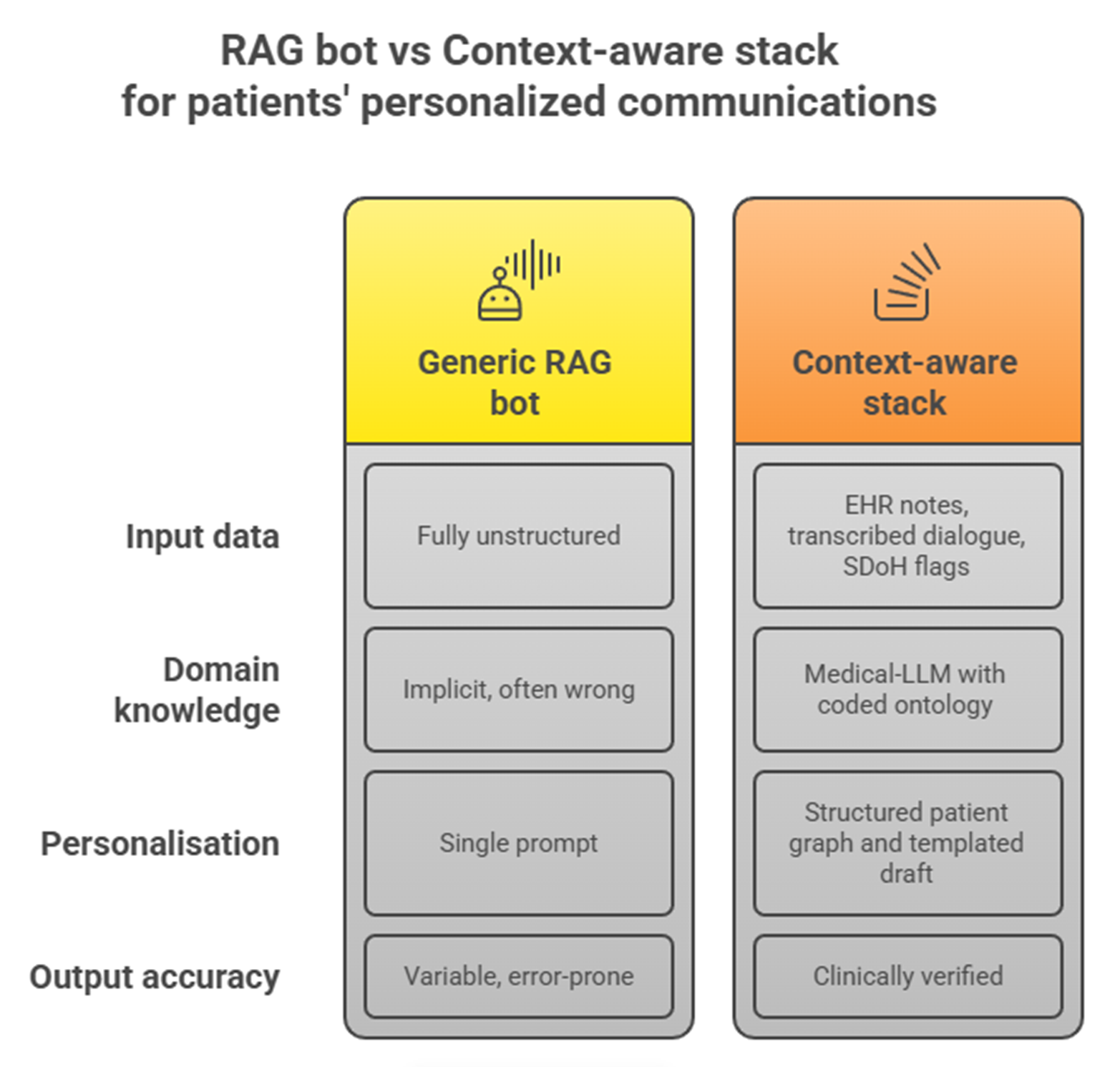
Comparison of a generic RAG bot versus a context-aware stack solution.
Most innovative projects now build on a stack that mixes a healthcare-ready large language model with specialized clinical natural language processing tools. John Snow Labs provides that stack so teams can create end‑to‑end messaging solutions in the most efficient way.
Typically, these systems rely on a common architecture that welcomes multiple data sources. Secure emails, portal chats, and even audio from scribes pass through Healthcare NLP. When a medical scriber system is in place, the WhisperForCTC component can load the whisper model to turn speech into text with high accuracy, so a remark from Julia like “I skipped breakfast because my food cupboard is empty” is captured, coded, and integrated into a knowledge base about her within seconds.
The pipeline usually starts by sending free text, Continuity‑of‑Care Documents, clinical notes, transcriptions from dialogues, or portal messages through ner_jsl_enriched. For Julia, this single step finds her conditions (“diabetes,” “high blood pressure”), her drugs (“metformin 500 mg,” “lisinopril 10 mg”), and lifestyle clues such as “trouble climbing stairs” or “short on food money.” Another model for Social Determinants of Health tags phrases like “fixed income” and “lives alone.” Assertion detection then marks each finding as current, ruled out, or past, preventing outdated facts from re‑appearing.
An especially useful model when dealing with patient communication is the so-called Voice of the Patients. Being tuned to phrases that people use in daily life, it spots words like “water pill” for diuretic, “puffer” for inhaler, or “light-headed” instead of vertigo and tags each with the right clinical concept.
Next, the system adds codes. A resolver maps “HbA1c” to its LOINC code and “metformin” to its RxNorm code so automated rules can link price data or benefit checks. Procedures gain CPT codes that billing systems already recognize.
Quality safeguards operate early. A medical spell checker cleans typing errors in portal notes, and a de‑identification pipeline masks personal identifiers before logs reach storage, protecting privacy regulations.
With the clinical graph in place, generation can begin. A medical‑tuned large language model, the 14B parameter Medical LLM that reads long documents and surpasses GPT-4 on several clinical benchmarks⁴, rewrites the message to the patient in clear language. Before the model drafts, a template engine can insert the facts: Julia’s precise pill schedule, directions to the closest food bank, and a safe‑exercise video designed for people with knee pain.
Personalized Communication for Julia
Hello Julia,
Your recent lab results show an A1C of 8.3 percent. Together we can bring this number down while easing the joint pain in your knees and working within your food budget. Below is a plan created from our recent conversation, the notes Dr. Morgan dictated, and the messages you sent last week about grocery costs and stair climbing.
This Week’s Focus
Morning routine: Take metformin 500 mg and lisinopril 10 mg with breakfast at 8 a.m. A gentle reminder will arrive on your phone ten minutes before.
Easy movement: Our physical‐therapy colleague selected a five-minute chair-exercise video suited to sore knees. A link appears in your portal every other day at 9 a.m.
Smart shopping: Because the nearest full grocery store is four miles away, the community food market on Maple Street offers low-cost produce boxes on Fridays. We reserved one for pickup this week, and directions are included below.
Balanced meals: When breakfast feels rushed, try the oatmeal packet we discussed with a spoon of peanut butter for protein. This keeps sugar steady without added cost.
Glucose checks: Measure before lunch and at bedtime. Enter the numbers in the portal; the chart updates automatically so we can spot patterns.
Next Steps
Your annual foot and eye exams are scheduled for May 14. Transportation help is available if needed; just reply “ride” in the portal, and a coordinator will call within one business day.Remember, small steps add up. You have taken more consistent doses this month than at any time last year, and your home readings already show progress. We are here to encourage you at every turn.
Warm regards,
The Diabetes Care Team
City Health ClinicIMPORTANT NOTE: Communication generated with Healthcare NLP and medical language-model technology to ensure clarity and accuracy while reflecting your individual needs.
Targeted guidance that turns advice into action
Today, six months after that difficult appointment and the incorporation of a smart AI solution to personalize communications to patients, Julia checks her glucose log with quiet pride. The new messages arriving in her portal feel written with her, not at her, each one timed to her meals, matched to local food‑bank hours, and mindful of her arthritic knees. She no longer files the clinic email under “someday.” Pharmacy refill records and self‑reports show that she takes her medicines on schedule nine days out of ten, up from five before the change. Her nurse now spends visits celebrating small wins instead of revisiting basics. Clear, personal language turned guidelines into action, and Julia feels heard, supported, and in charge of her health journey.
References
[1] Zolnierek KB, Dimatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009 Aug;47(8):826-34. https://pmc.ncbi.nlm.nih.gov/articles/PMC2728700/ [2] Chan A, De Simoni A, Wileman V, Holliday L, Newby CJ, Chisari C, Ali S, Zhu N, Padakanti P, Pinprachanan V, Ting V, Griffiths CJ. Digital interventions to improve adherence to maintenance medication in asthma. Cochrane Database Syst Rev. 2022 Jun 13;6(6):CD013030. https://pubmed.ncbi.nlm.nih.gov/35691614/ [3] Nguyen M, et al. Context‑aware discharge instructions improve patient comprehension. Journal of Biomedical Informatics. 2024. https://pmc.ncbi.nlm.nih.gov/articles/PMC12122782/ [4] Rajpurkar P, et al. Identifying social risk from clinical notes with large language models. npj Digital Medicine. 2025. https://www.nature.com/articles/s41746-025-01645-8 [5] John Snow Labs. Medical Large Language Models – 2025 release. https://nlp.johnsnowlabs.com/docs/en/LLMs/medical_llm