Why data de‑identification is not optional in healthcare AI
In healthcare AI, the cornerstone isn’t just smart models. It’s trusted data. Without rigorous de‑identification and governance, any AI initiative risks regulatory violation, data breach, or re‑identification exposure. Put plainly: if your data is not de‑identified (or properly pseudonymised and governed), you don’t have an AI strategy, you have a liability.
What are the core risks of insufficient data de‑identification
- Regulatory non‑compliance: Laws like HIPAA, GDPR, and emerging jurisdictions enforce strict rules on processing identifiable health data; penalties, delays, and audits follow mis‑steps.
- Re‑identification threat: Modern linking techniques (image + metadata + clinical text) make naive de‑identification insufficient; weak masking may allow re‑linking to individuals.
- Data breach and reputational damage: Health data is highly sensitive; a breach not only harms patients but destabilizes institutional trust and can damage AI adoption.
- Operational paralysis: If data pipelines are blocked by compliance fears or manual review burdens, AI workflows fail before even launching.
How to engineer a robust de‑identification strategy
- Define the de‑identification scope and target use‑cases
- Classify data types: structured EHR, free‑text clinical notes, imaging metadata, genomics.
- Determine whether full anonymisation, pseudonymisation or controllable synthetic data is required based on downstream use‑cases (research, model training, production inference).
- Map data sources and flows.
- Build an auditable, automated de‑identification pipeline
- Use tools that support entity recognition (names, dates, identifiers), context‑aware masking, metadata sanitization, and consistent tokenization across visits.
- Ensure imaging metadata (DICOM headers), clinical notes (PHI in free text) and cross‑linkage between modalities are addressed.
- Generate audit trails: what was masked, how, when, by whom; maintain logs for compliance and model governance.
- Apply model‑ready transformations while preserving data utility
- Balance between de‑identification and utility: retain clinical semantics, temporal relationships and cohort fidelity while removing re‑identification risk.
- Use pseudonymization when linkage across encounters is required for longitudinal modeling, but apply governance around re‑linking keys.
- Leverage synthetic data augmentation or differential‑privacy techniques in selected cases.
- Integrate governance, monitoring and human oversight
- Define roles: data stewards, compliance officers, AI governance boards.
- Monitor de‑identification performance: measure residual risk, external validation, re‑identification testing.
- Embed human‑in‑the‑loop checks, especially for free‑text and edge‑cases (e.g., rare diseases, small cohorts).
- Prepare for downstream AI pipelines and auditability
- Ensure traceability from raw data through processing to model input and output; document versioning and transformations.
- Connect de‑identification logs to model governance systems, so any model output can trace back to input cohort and masking logic.
- Develop incident response and breach protocols: if re‑identification occurs or data leak happens, remediation and notification must be defined.
How John Snow Labs supports data de‑identification in healthcare
John Snow Labs offers advanced tools and frameworks tailored for healthcare de‑identification and governed AI:
- Comprehensive clinical‑text de‑identification models which identify PHI entities (names, dates, providers, locations) and provide mask
- ing/pseudonymization pipelines.
- Additional anonymization methods beyond masking, as consistent obfuscation methods that reduce the probability of false negatives spotting by an attacker while preventing information loss in real world evidence (RWE) applications.
- Image metadata sanitization and DICOM header cleaning capabilities integrated into data ingestion pipelines, ensuring imaging datasets are PHI‑safe before model training.
- Audit‑ready processing logs, pipeline orchestration, human‑in‑the‑loop correction workflows and integration with enterprise data platforms (Healthcare NLP) so that masking and traceability are baked into production pipelines.
- Governance frameworks and best‑practice playbooks aligning with HIPAA, GDPR and AI regulatory regimes, enabling organizations to deploy AI with confidence rather than fear.
What happens if you skip the de‑identification layer?
- AI projects stuck in “data sandbox” stage because production pipelines can’t access identifiable data safely.
- Regulatory audits uncover insufficient masking and models are disqualified from marketplace or forced offline.
- During model training and evaluation you have access to less data leading to biased or non‑generalizable results, undermining trust.
- Data breach or re‑identification event triggers not only penalties but erodes clinician, patient and stakeholder confidence, undermining all downstream AI investment.
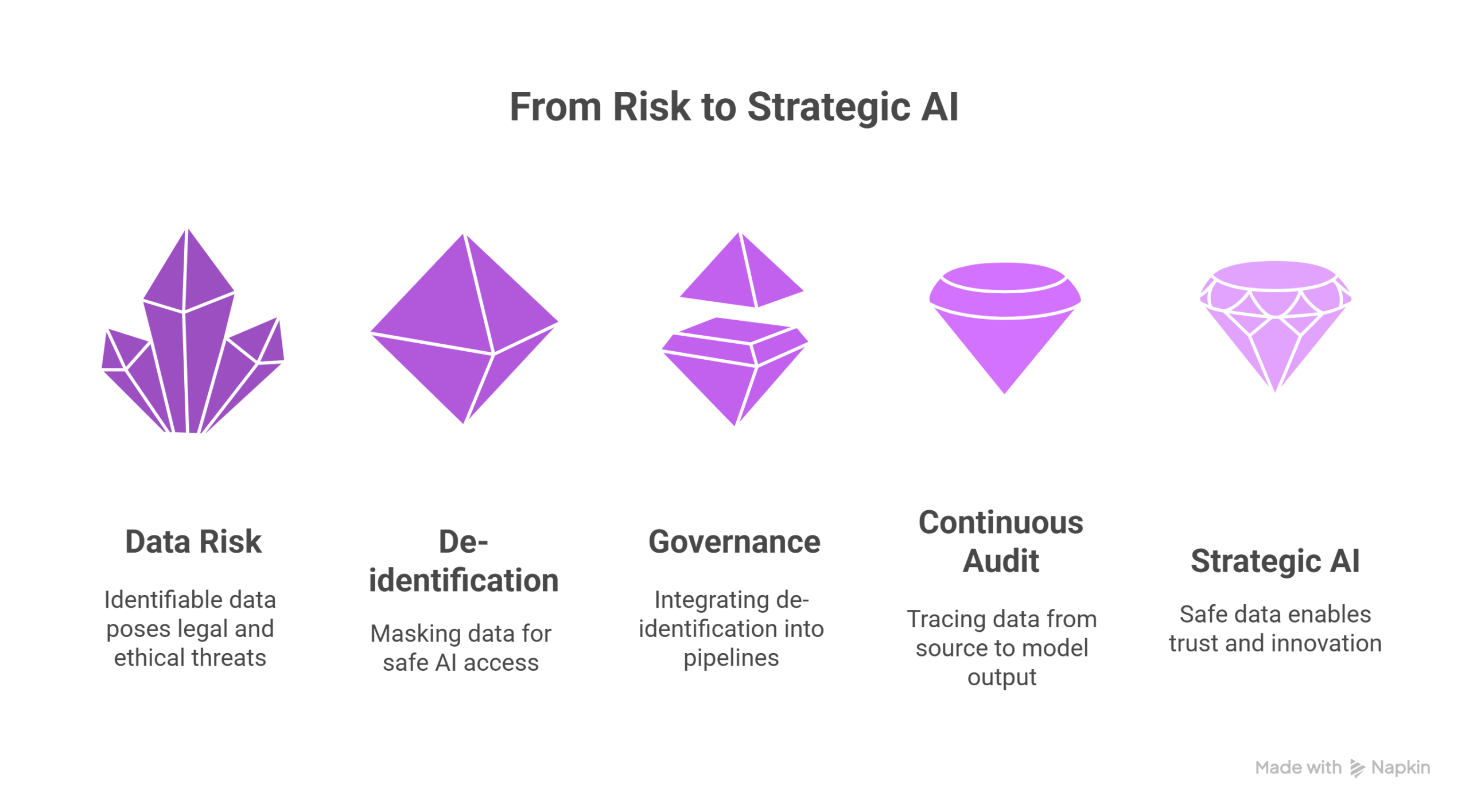
Conclusion: De‑identification is the foundation of your AI strategy
No matter how advanced your models or clever your use‑cases, without robust de‑identification and governance, you lack a viable AI strategy. The organizations that succeed will treat de‑identification as core infrastructure, integrate it into data pipelines, audit continuously and trace from source to model output.
With John Snow Labs’ de‑identification frameworks, masking pipelines and governance ecosystem, you can shift from risk‑avoidance to strategic‑enablement of AI. In healthcare, the first step in the AI journey is safe data. Because without it, everything else is built on sand.
FAQs
Q: Can synthetic data replace de‑identification?
A: Synthetic datasets can supplement but not fully replace robust de‑identified real‑world data, especially for clinical modelling. De‑identification and synthetic augmentation often go hand‑in‑hand.
Q: How do you measure re‑identification risk?
A: Techniques include k‑anonymity, l‑diversity, membership‑inference testing, external linkage attack simulations, and governance audits of pipeline logs and divergence metrics.