In a busy hospital in the Midwest, a nurse reviewing patient notes notices a pattern: a middle-aged man admitted for pneumonia had also reported mild dizziness and blurred vision during previous visits. An AI powered system flags a potential adverse drug reaction – one that hadn’t been documented in structured fields. Within hours, the care team adjusts his medication, potentially preventing a serious complication.
This is not fiction, it’s what predictive analytics, powered by natural language processing (NLP) and large language models (LLMs), is beginning to enable in real-world clinical settings. And while technology is promising, the road to widespread adoption still involves bridging technical, operational, and cultural gaps.
Why patient’s safety require a new lens?
Adverse events are among the most preventable harms in healthcare, yet they remain all too common. Approximately 1 in 10 hospitalized patients worldwide experiences one, often due to medication interactions, delayed diagnoses, or overlooked comorbidities¹.
Traditional methods for identifying these events, like chart audits or clinician self-reporting, are slow and incomplete. They tend to capture what’s already gone wrong, not what might go wrong next. That’s where predictive analytics, particularly when integrated with Healthcare NLP, shifts the focus from reaction to anticipation.
Turning notes into signals: How does Healthcare NLP work?
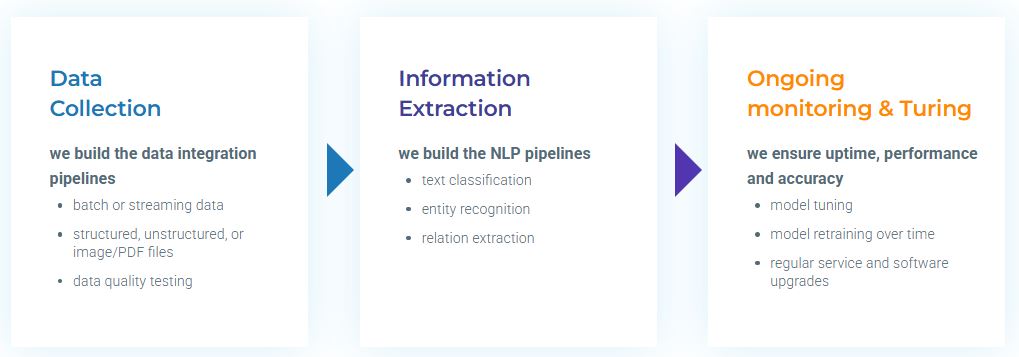
Unstructured clinical notes hold rich insight. But they’re often overlooked by traditional analytics. Healthcare NLP by John Snow Labs makes these notes legible to machines and useful to humans.
Take John Snow Labs’ Adverse Drug Reaction (ADR) Detection Model. It processes free-text notes to identify drug-event relationships. More importantly, it understands context, discerning between phrases like “the patient denies chest pain” and “chest pain reported last night.” This matters. It avoids false alarms and focuses attention where it’s truly needed.
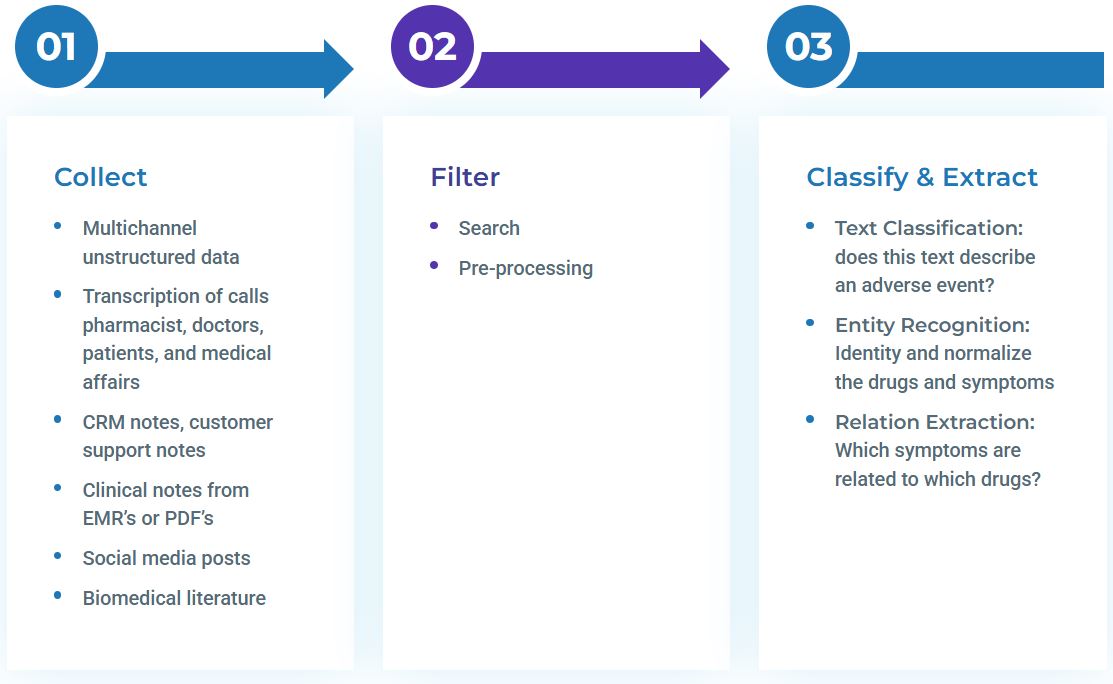
Behind the scenes, three core technologies do the heavy lifting:
- Named Entity Recognition (NER): Extracts key terms like symptoms and medications.
- Relation Extraction: Connects the dots between cause and effect.
- Assertion Status Detection: Distinguishes between confirmed, negated, and hypothetical mentions.
Why does culture matter as much as code?
Technology doesn’t operate in a vacuum. Research shows that organizations with stronger patient safety cultures experience fewer reported adverse events2. In fact, nine different safety culture dimensions were associated with a lower perception of adverse outcomes.
This suggests that successful implementation involves more than just deploying a model. It requires leadership buy-in, clinician training, and a shared commitment to learning from data.
How have we progressed and what is coming in the next years?
There are signs of progress. Between 2010 and 2019, in-hospital adverse event rates declined significantly for certain conditions, including myocardial infarction and major surgeries. But for most other diagnoses, the rate has stubbornly held at 70 adverse events per 1,000 discharges3.
The takeaway? While predictive tools are gaining ground, meaningful impact still requires broader innovation in care design, data governance, and organizational readiness.
What do healthcare leaders need to know?
Predictive analytics is not a cure-all, but it is a powerful enabler. For CMIOs and care quality leaders, it can augment surveillance efforts and elevate care precision. For CIOs and CISOs, platforms like Healthcare NLP offer a compliant, secure foundation for scalable AI integration.
Crucially, the most effective implementations are those that align technological innovation with human factors, trust, transparency, and the realities of clinical decision-making.
From alert to intervention: What happens next?
As the nurse in our opening story discovered, predictive analytics doesn’t just surface risk, it opens a door to timely action. But to walk through that door, organizations need not just algorithms, but alignment: between departments, between systems, and between aspiration and reality.
The potential is there. And when prevention matters most, every signal, when seen in time, can make a difference.
Dive deeper: Read our newest articles on AI in healthcare.
References:
[1] World Health Organization. Patient Safety: Making Health Care Safer. https://www.who.int/news-room/fact-sheets/detail/patient-safety
[2] Agency for Healthcare Research and Quality (AHRQ). Patient Safety Culture Surveys. https://www.ahrq.gov/sops/index.html
[3] Agency for Healthcare Research and Quality (AHRQ). 2023 Chartbook on Patient Safety. https://www.ahrq.gov/research/findings/nhqrdr/chartbooks/patientsafety/index.html