Introduction
In today’s fast-paced healthcare environment, clinicians face a mounting challenge: balancing patient care with the overwhelming administrative tasks of documentation. SOAP notes, a standardized method developed by Dr. Lawrence Weed in 1968, are essential for recording patient encounters. However, their manual creation consumes precious time and often leads to errors, contributing to clinician burnout.
By leveraging medical language models and integration with platforms like AWS HealthLake and Amazon SageMaker, John Snow Labs is addressing the inefficiencies of manual documentation. This blog will explore the technology behind automated SOAP notes, its practical applications, and its impact on patient care and workflow efficiency.
The Problem: Manual SOAP Notes Are Inefficient
Manual SOAP notes are not just time-consuming but also prone to errors. Here’s why:
- Time Consumption:
- Documentation Errors:
- Documentation issues play a role in 10–20% of medical malpractice lawsuits, often due to inaccurate or incomplete records.3
- Clinician Burnout:
- Excessive documentation demands contribute significantly to clinician burnout, reducing the quality of patient interactions and overall job satisfaction.
- Legal and Compliance Risks:
- As legal documents, SOAP notes must be accurate. Errors can result in liability issues and affect insurance audits.
The Solution: Automating SOAP Notes with AI
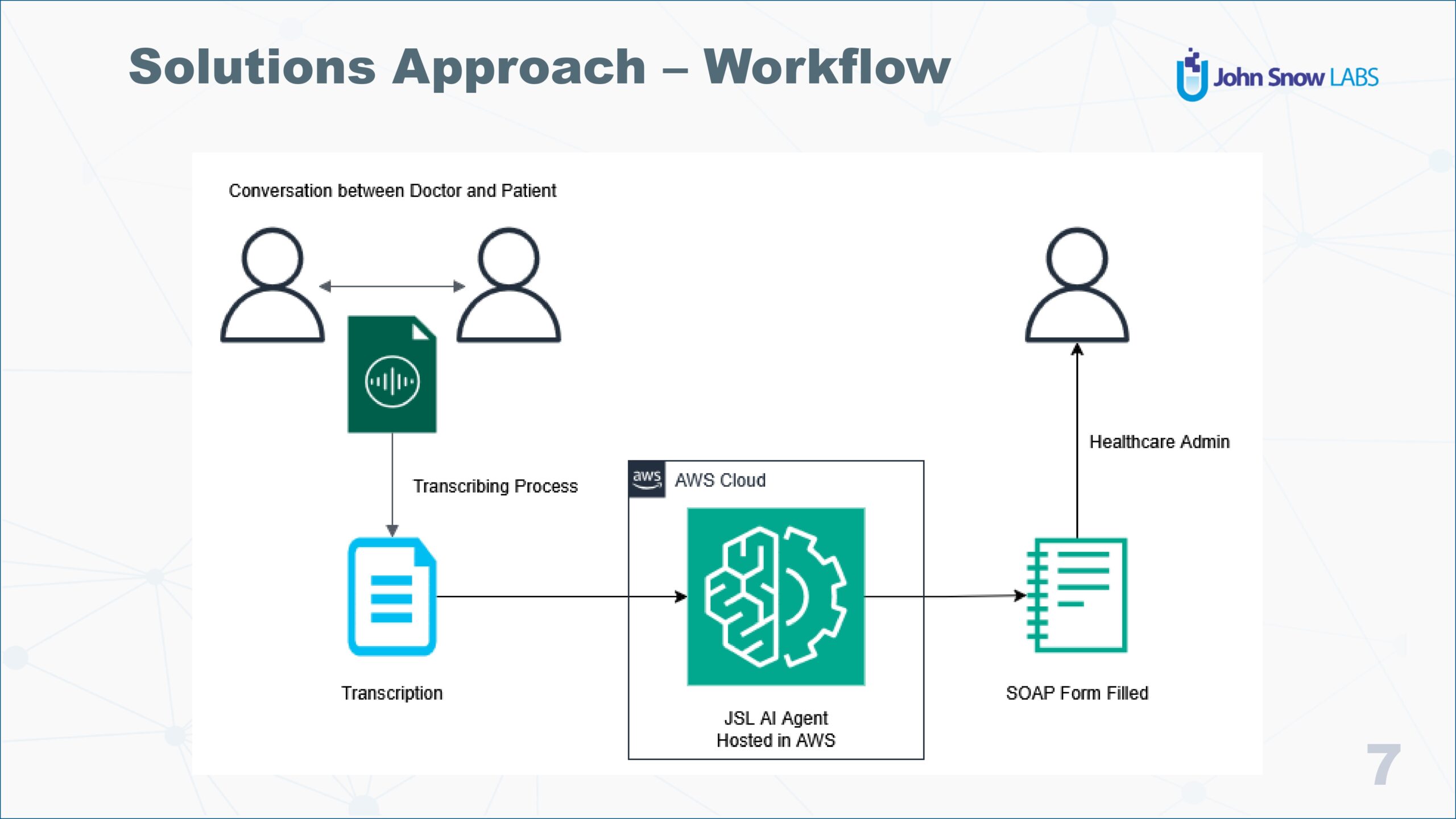
John Snow Labs, in collaboration with Amazon Web Services (AWS), offers an innovative solution to automate SOAP note generation. The Medical LLMs from John Snow Labs streamline documentation by leveraging Natural Language Processing (NLP) and advanced machine learning techniques.
How It Works:
- Data Capture:
- AI agents extract data from various sources like voice recordings, transcripts, and EHRs.
- Integration with AWS services ensures secure and compliant data handling.
- Automated Note Generation:
- NLP models convert raw input (e.g., audio or text) into structured SOAP notes.
- The system identifies key components (Subjective, Objective, Assessment, Plan) and populates the template automatically.
- Real-Time Validation:
- The model cross-references data to minimize errors, making real-time adjustments as necessary.
- Seamless Integration:
- Works with existing EHR systems like Epic and Cerner, eliminating the need for retraining staff.
Key Technology Stack
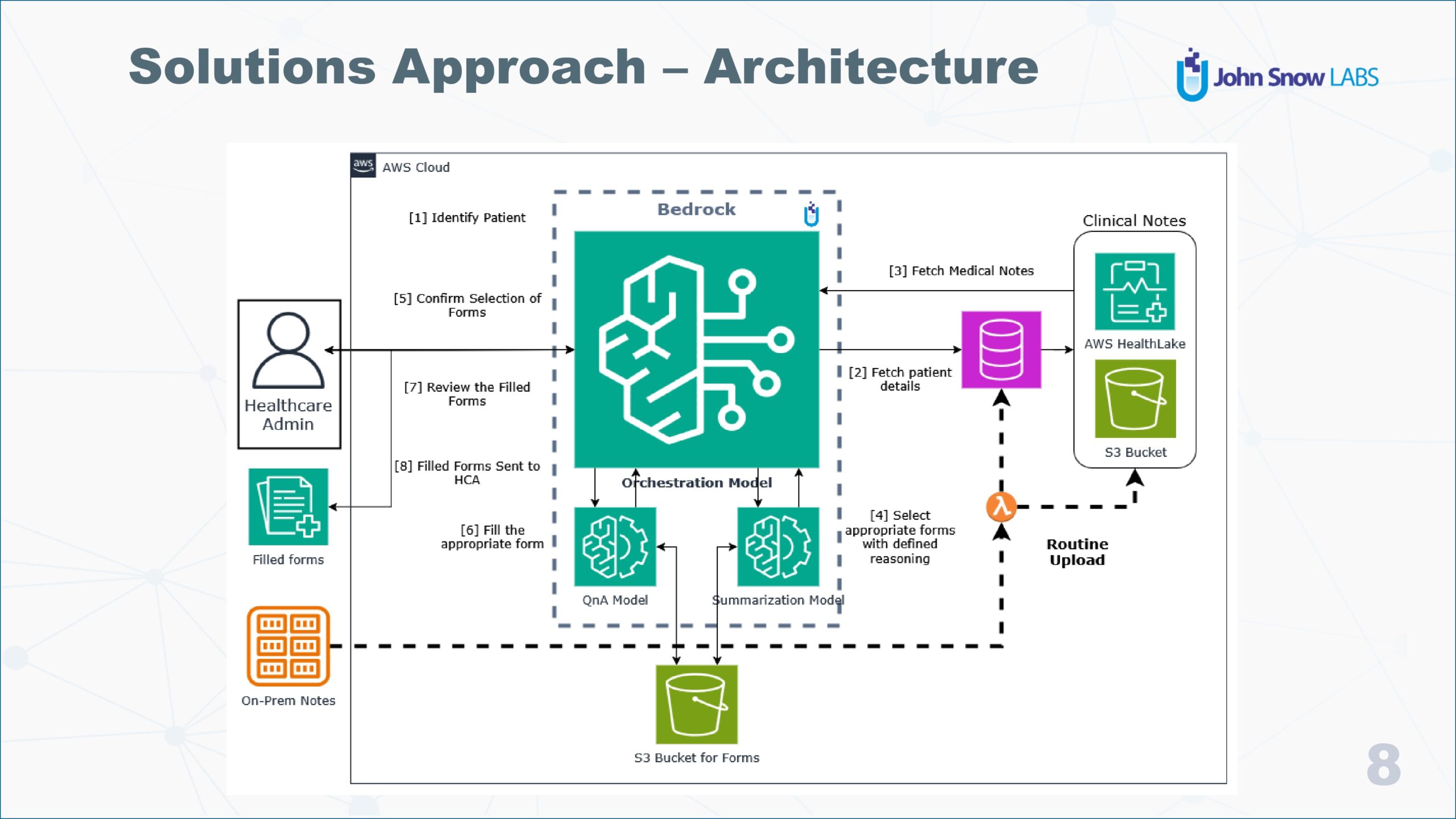
The backbone of automated SOAP note generation lies in integrating AI models with robust AWS infrastructure.
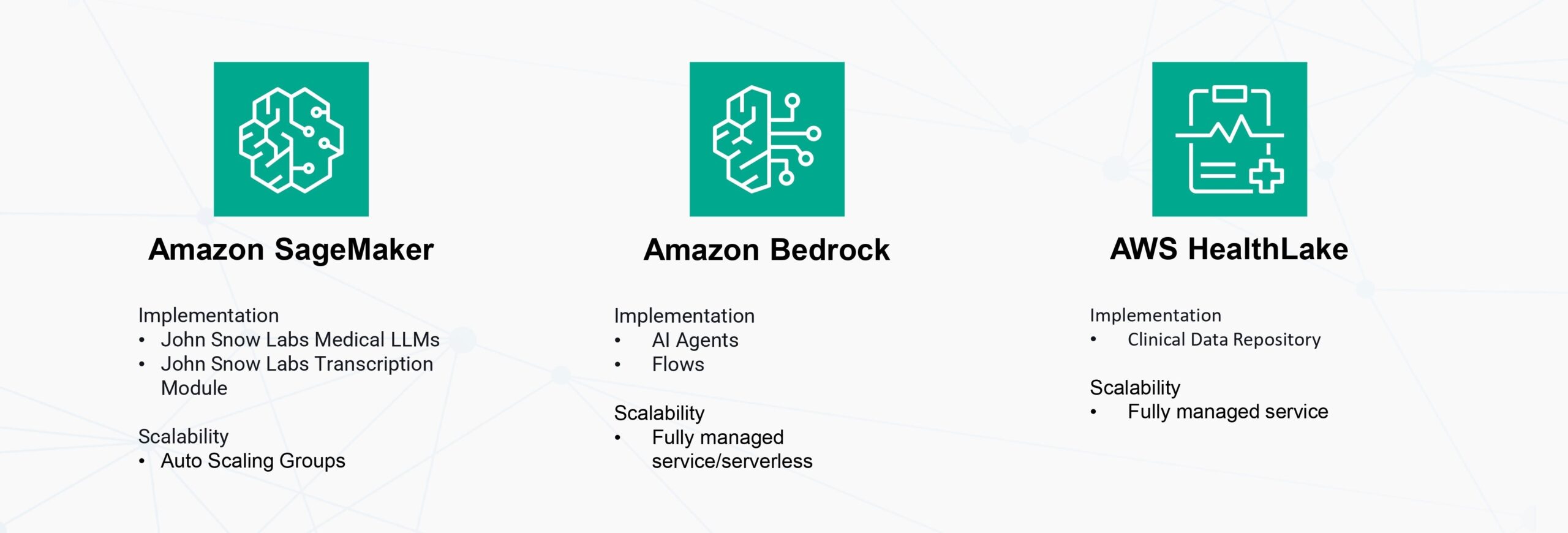
The power behind the seamless automation of SOAP note generation lies in a sophisticated integration of AI models with a reliable and scalable cloud infrastructure, notably through AWS (Amazon Web Services). At the heart of this innovation is AWS HealthLake, a clinical data repository that acts as a vital tool in transforming the way
healthcare data is handled. HealthLake’s ability to process and organize unstructured health data is nothing short of revolutionary, converting it into a structured, searchable format that can be easily navigated by clinicians and healthcare systems alike. This transformation not only improves data accessibility but also ensures that healthcare organizations remain in compliance with rigorous regulations, addressing the unique needs of the healthcare industry while upholding strict privacy and security standards.
On top of HealthLake’s capabilities, Amazon SageMaker plays a crucial role in deploying machine learning models at scale. This powerful tool supports both real-time and batch processing of SOAP notes, offering flexibility to accommodate the varied needs of healthcare settings. Whether handling a steady stream of patient data or processing large batches of records at once, SageMaker’s auto-scaling capabilities ensure that the system adapts to fluctuating data loads, maintaining optimal performance at all times. This adaptability is essential for keeping up with the ever-growing volumes of patient information that healthcare systems must manage.
To further enhance the capabilities of automated SOAP note generation, Amazon Bedrock provides the foundational framework for autonomous AI agents. Bedrock supports complex AI workflows through its innovative flow management system, ensuring that the automation of SOAP notes runs smoothly and efficiently. It also integrates seamlessly with John Snow Labs’ Medical LLMs (Large Language Models), enabling the AI agents to understand and process medical language with incredible accuracy. This integration ensures that the automated system is not only efficient but also highly capable of delivering precise, contextually relevant SOAP notes in a fraction of the time it would take a clinician to document manually.
Together, these powerful AWS tools—HealthLake, SageMaker, and Bedrock—create a robust and dynamic infrastructure that powers the future of healthcare documentation, ensuring that clinicians can focus more on patient care while benefiting from streamlined, accurate, and compliant documentation processes.
 Real-World Impact
Real-World Impact
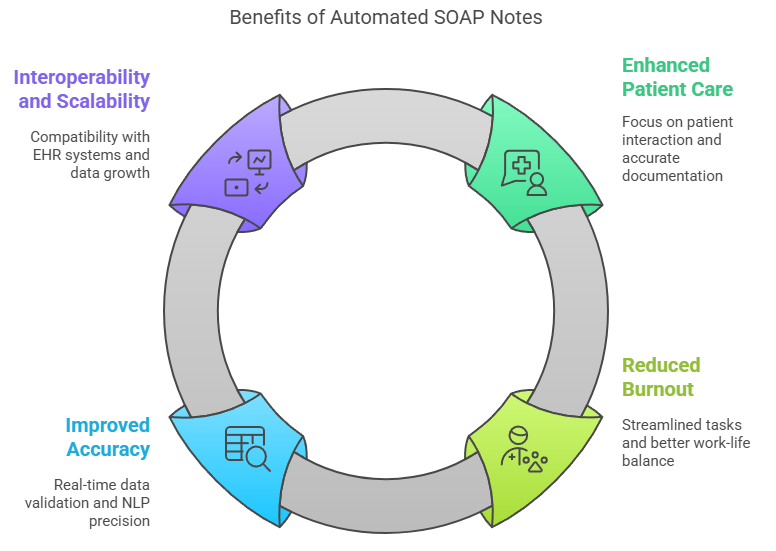
In the fast-paced and high-pressure world of healthcare, the constant balancing act between patient care and administrative duties has always posed a challenge. However, recent advancements in technology are providing much-needed relief, offering clinicians tools that can transform the way they manage both their time and their responsibilities. One such advancement is the automation of SOAP notes, which is playing a pivotal role in enhancing patient care. Traditionally, SOAP notes — the cornerstone of clinical documentation — can consume a significant portion of a clinician’s time, often at the expense of direct patient interaction. By automating these notes, clinicians are freed from the burden of paperwork, allowing them to redirect their attention to what truly matters: their patients. This shift not only improves the quality of patient care but also ensures that documentation is timely and accurate, helping to reduce the risk of clinical errors that could otherwise have serious implications.
This automation also serves a critical role in reducing clinician burnout, a growing issue within the healthcare industry. Administrative overload has long been a contributor to burnout, with clinicians often feeling overwhelmed by the sheer volume of paperwork and non-clinical tasks. By streamlining these administrative responsibilities, the automation of SOAP notes significantly lightens the workload for healthcare professionals. The result is not only a more manageable day-to-day schedule but also a stronger foundation for a healthier work-life balance. Clinicians can spend more time on meaningful patient care and less time navigating the complexities of documentation, which ultimately contributes to their overall well-being.
Furthermore, the integration of real-time data validation and context-driven natural language processing (NLP) technology ensures improved accuracy in clinical documentation. These sophisticated systems continuously check for precision and completeness in SOAP notes, providing clinicians with immediate feedback to ensure the highest standards of documentation. This real-time validation minimizes the chances of errors that could lead to serious consequences, such as malpractice claims. By ensuring that each note is both thorough and accurate, this technology plays a vital role in safeguarding patient safety and the clinician’s professional integrity.
Another significant benefit of automated SOAP notes is their interoperability and scalability. Designed to seamlessly integrate with leading electronic health record (EHR) systems, this technology minimizes disruption to existing workflows. Clinicians can adopt the new system without having to completely overhaul their processes, which helps smooth the transition and accelerates adoption. Moreover, as the volume of patient data continues to grow, the automated system scales efficiently to handle increasing amounts of information without compromising on performance or accuracy.
In sum, the automation of SOAP notes offers a transformative solution for healthcare professionals. By enhancing patient care, reducing burnout, improving accuracy, and ensuring compatibility with existing systems, it allows clinicians to focus more on their patients and less on administrative burdens. The result is a more efficient, accurate, and supportive environment for healthcare delivery, benefiting both patients and clinicians alike.
Use Cases and Success Stories
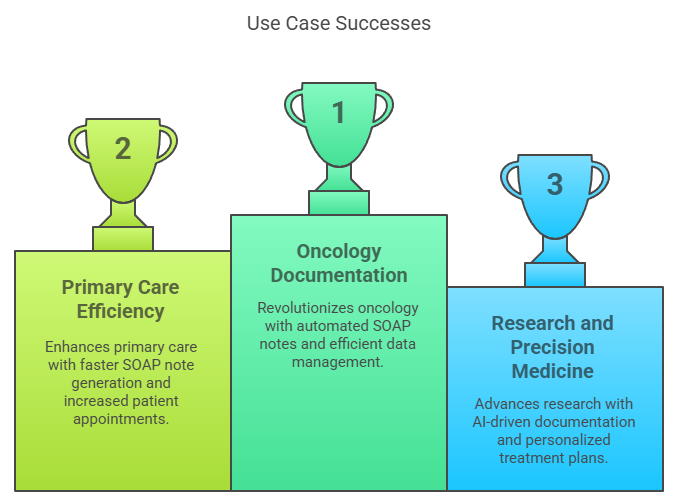
In the specialized field of oncology, managing complex patient data is a critical and time-consuming task that demands precision and efficiency. Automated SOAP notes are proving to be a game-changer for oncologists, helping them efficiently handle the vast amounts of information involved in patient care. These notes significantly reduce the time spent reconciling imaging and text reports, which is traditionally a cumbersome process. By streamlining this aspect of documentation, oncologists can make quicker, more informed decisions about patient treatment plans, ultimately improving the quality of care and accelerating response times to evolving patient needs.
Similarly, in primary care settings, the benefits of automated SOAP notes are becoming increasingly evident. The ability to generate SOAP notes faster enables primary care physicians to see more patients within the same timeframe, enhancing the overall flow of daily operations. By reducing the time spent on note-taking, these automated systems increase clinic productivity, allowing healthcare providers to focus more on patient interaction and less on administrative tasks. This improvement in efficiency is not only beneficial for clinicians but also helps patients by reducing wait times and increasing the number of appointments available each day.
Beyond day-to-day patient care, automated documentation is also having a profound impact on research and precision medicine. AI-driven systems play a key role in facilitating the analysis of vast amounts of patient data, which is essential for developing personalized treatment plans. By automating the documentation process, clinicians are able to access and analyze data more quickly and accurately, empowering them to create tailored therapies that address the unique needs of each patient. Moreover, automated documentation enhances the ability to track longitudinal patient data, which is crucial for observing the progression of diseases and adjusting treatments over time. This capability is particularly valuable in the context of precision medicine, where a comprehensive understanding of a patient’s health history is vital for making informed, evidence-based decisions.
In sum, the automation of SOAP notes is not just a time-saving tool—it is transforming oncology care, improving primary care efficiency, and advancing research and precision medicine. By enabling faster, more accurate documentation, healthcare professionals are empowered to make better decisions, see more patients, and provide personalized care that is based on real-time data and analysis.
Addressing Common Concerns
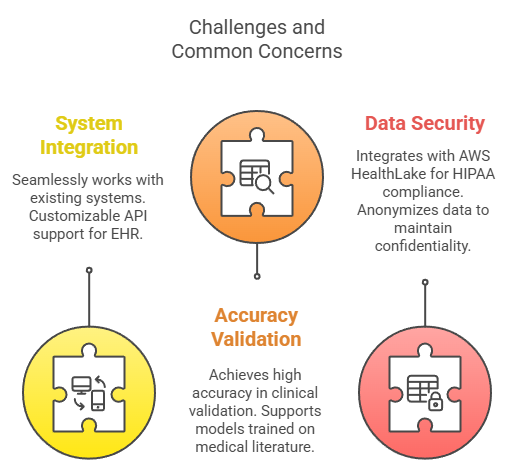
Incorporation of generative AI modules in clinical environments often starts with the same question: Will this actually fit into what we already use? That’s why Integration with existing systems is so important. This tool doesn’t force clinicians or IT teams to start from scratch. It connects smoothly with established platforms like Epic and Cerner, meaning there’s no need for extra training or complicated setup. For those working in different environments, a flexible API is available, making it adaptable to a wide range of electronic health records.
But ease of use wouldn’t matter much if the tool wasn’t dependable. That’s where accuracy and validation come in. In clinical settings, it’s reached accuracy rates of over 95%, a figure that’s not just for show, it comes from solid validation studies. It also uses models grounded in peer-reviewed research and real-world patient cases, which helps build trust among healthcare professionals who rely on clear and precise information.
Of course, in any medical setting, protecting patient data is non-negotiable. Data security and compliance is built into the system from the ground up. It connects with AWS HealthLake to stay in line with HIPAA rules, ensuring all personal health information remains secure. Even as data is being processed, it’s automatically anonymized, keeping identities safe while still allowing the system to learn and deliver helpful insights.
Conclusion
Automating SOAP notes with AI is a game-changer for healthcare professionals, improving both efficiency and patient outcomes. By integrating advanced NLP models with AWS infrastructure, John Snow Labs provides a reliable, scalable solution tailored to the needs of modern healthcare settings.
For more information on John Snow Labs Medical LLMs and implementation guidance, visit: https://www.johnsnowlabs.com/healthcare-llm/
For more information on implementing AI agent solutions on AWS refer to: https://docs.aws.amazon.com/bedrock/latest/userguide/agents.html
[1] S. Ayele, T. Gobena, S. Birhanu, and T. A. Yadeta, “Attitude towards documentation and its associated factors among nurses working in public hospitals of Hawassa City Administration, Southern Ethiopia,” SAGE Open Nurs., vol. 7, p. 23779608211015363, May 2021, doi: 10.1177/23779608211015363 [2] A. Cass, “The hours 23 physician specialties spend on paperwork, administration,” Becker’s Hospital Review, Apr. 19, 2023. [Online]. Available: https://www.beckershospitalreview.com/quality/hospital-physician-relationships/the-hours-23-physician-specialties-spend-on-paperwork-administration/ [3] S. Ghaith, G. P. Moore, K. M. Colbenson, and R. A. Lindor, “Charting practices to protect against malpractice: Case reviews and learning points,” PMC, vol. 2022, Article ID PMC9183775, doi: 10.1136/j. med. 2022.35679491























 Real-World Impact
Real-World Impact